Almost 1 in 5 breast cancer patients who have undergone breast cancer treatments develop lymphedema. Lymphedema is a chronic complication of breast cancer treatment. Usually it occurs within weeks of treatment and subsides on it's own.But it can occur at anytime in the lifetime of breast cancer treated patient and if not prevented or treated early , it can be permanent and hampers the quality of life of a successfully treated breast cancer patient.
What is breast cancer treatment-related lymphedema ( BCRL):
Lymph is clear watery fluid that drains out from the blood capillaries into body tissues. The major functions of lymph are as follows:
- Drains out the extra fluid consisting of toxins and other waste products, formed due to metabolism between the cells into blood stream.
- Lymph helps in absorbing the fats and proteins from small intestine by transporting it to blood stream.
- Lymph also contains white blood cells that form the immune system of the body to fight again infections.
Because of breast cancer or breast cancer treatments ( surgery and radiation therapy ) the fluid drainage channels of lymphatic system are hampered and the lymph fluid can not be drained out quickly and start getting accumulated causing the area to swell causing lymphedema. Lymphedema can develop in the arm or hand of the affected side. It can also develop in chest,breast,shoulder,trunk or on the back
If Lymphedema is not treated in time it can get worse. It can be painful and moving the affected arm or hand will be difficult.
Signs and symptoms of Lymphedema:
Lymphedema may have a slow onset of swelling in the arm , hands or fingers of the affected side or it could be acute too.
An unusual sensation in the hand of the affected side , usually numbness or tingling even before the swelling is noticeable.
Symptoms of lymphedema post breast cancer treatment may include:
- A recent change in skin either in appearance or texture such as itching , tightness, redness , rash or tightening.
- Feeling of discomfort , achiness , tingling or increased warmth in affected area hand , chest, breast or underarm.
- Feeling fulness or heaviness in affected area arm , chest , breast , underarm, shoulder or back.
- Tightness or difficulty in moving shoulder , hands and wrists.
- tenderness in the elbow
- Burning or shooting pain sensations that may seem like pricking with pins and needles.
- Slight puffiness or swelling in arm, hand, breast, or chest with a temporary indentation of the skin when one presses on it with one's finger (this is called pitting edema).
- Veins or tendons in the hand that are harder to see, knuckles that look less pronounced, or once-wrinkled skin that looks smoother.
- Fever or flu like symptoms
If one observe a sudden swelling in the arm , hand , chest , breast or underarm , one must seek medical attention asap as it may indicate an infection, a blood clot (also known as deep vein thrombosis), or cancer recurrence that is affecting the lymphatic system.
What are risk factors associated with breast cancer treatment related lymphedema:
Breast cancer surgery as causative factor for lymphedema:
Surgery is the mainstay for breast cancer treatments. Breast cancer surgery involves removal of either the whole breast ( Mastectomy ) or removal of the tumor or lump
( Lumpectomy ) along with involved lymph nodes specially the axillary lymph nodes in the armpit area. But a breast cancer surgery may also cause lymphedema in breast cancer patients. Your breast cancer surgeon and healthcare professionals will advise you the preventive measures to avoid lymphedema post breast cancer surgery.
An extensive breast surgery for treating breast cancer can disturb the lymph drainage channels of lymphatic system and may become a causative factor for lymphedema. Total mastectomy as compared to lumpectomy increases the risk more.
Axillary lymph node dissection ( ALND) largely determine a breast cancer patient's risk of developing breast cancer treatment related lymphedema ( BCRL).
Both extensive axillary lymph node dissection ( ANLD) as well as less extensive Sentinel lymph node biopsy ( SLNB) increases life long risk of developing breast cancer related lymphedema ( BCRL) in breast cancer patients.
Sentinel lymph node biopsy ( SLNB) is an effective option for staging the axilla while minimizing the risk of lymphedema in patients with clinically node negative breast cancer patients.
A lack of breast reconstruction post breast cancer surgery also increases risk of developing BCRL.
Breast cancer radiation therapy as causative factor for BCRL:
Radiation treatments for breast cancer can affect the lymphatic system. Scar tissue from radiation therapy may press on or narrow the lymph vessels and nodes that remain after breast cancer surgery. This damage interferes with the flow of lymph out of the arm and upper body.
Regional lymph node radiation ( RLNR) is also a causative factor for breast cancer treatment related lymphedema ( BCRL).
Regional lymph node radiation ( RLNR ) either supraclavicular with or without posterior axillary boost significantly increased the risk of breast cancer treatment related lymphedema risk compared to breast or chest wall radiotherapy alone.
Lack of breast reconstruction post breast cancer surgery as a causative factor for BCRL:
Mastectomy ( total removal of cancer affected breast ) itself is a major risk factor for breast cancer treatment related lymphedema , recent studies suggest that patients who have not undergone a breast reconstruction surgery post breast cancer surgery stand a higher chance of developing breast cancer treatment related lymphedema.
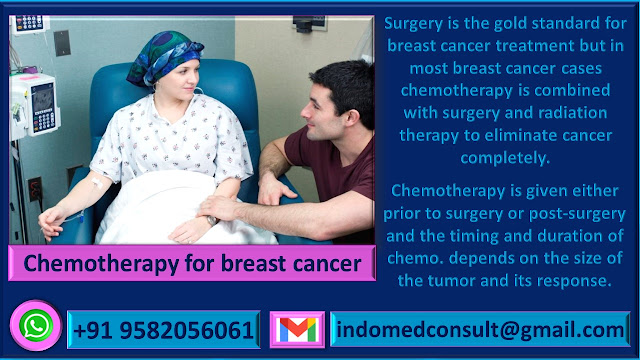
Chemotherapy induced breast cancer treatment related lymphedema:
Chemotherapy for treatment of breast cancer can be given both prior to breast cancer surgery or post breast cancer surgery. Certain breast cancer treatment chemotherapy protocols involving taxanes ( paclitaxel or docetaxel ) are also associated with increased risk of breast cancer treatment related lymphedema.
Intravenous chemotherapy may increase lymphedema risk if it’s placed in the arm on the same side of breast cancer surgery and lymph nodes removal.If chemotherapy is given IV through the pick line , it should be given from the opposite arm.Any picking with a syringe either to collect blood samples or administration of an Intravenous medication must also be done from the opposite arm of surgery side. It is advisable to give chemotherapy for treating breast cancer through a chemo port ( a small implantable device that is put in the upper chest area below the collar bone and under the skin ). It is used to draw blood and give treatments — including chemotherapy drugs — without a needle stick. A chemo. port can remain in place for weeks, months or even years.
Obesity and living a sedentary life style as a causative factor for BCRL:
People who live a sedentary life style and are obese ( overweight ) are more prone to develop breast cancer treatment related lymphedema post breast cancer treatment.
Sometimes the extra fat in obese women put pressure on lymph nodes and vessels and consequently disturbs the lymphatic system channels. Any disturbance in lymphatic system channels hampers lymph flow and drainage and thereby fluid build up takes place causing lymphedema.
Eating healthy and doing regular and suitable physical activities ( exercises ) not only keeps your weight in check but also reduces the risk of developing BCRL.
Any injury or infection can flare up BCRL:
A breast cancer patient may have fewer lymph nodes due to breast cancer surgery and any injury or infection can cause inflammation to body tissues. This inflammation may make the lymphatic system work harder because of increased blood flow and lymph fluid.
When one's lymphatic system can not cope up with this increased blood flow and lymph fluid due to infection or injury , a lymphedema can occur or gets flared up.
Air travel as causative factor for BCRL:
Air travel specially long distance flights or changing to connecting flights may increase the risk of flare up of Breast cancer related lymphedema.
Although it is not proven but theoretically there is a strong possibility that the
hypobaric–hypoxic environment inside the aircraft,
coupled with low cabin pressure, and the protracted
reduced movement and dehydration experienced on
flights, might be
sufficient to incite or exacerbate breast cancer treatment related lymphoedema( BCRL).
How you can reduce risk of BCRL post breast cancer treatment:
- Taking good care of arm on the surgery side.Your breast cancer surgery team doctors will advise you to elevate the affected arm a few times a day for the first 24 to 48 hours after surgery. You will be advised when it is safe to prop up the affected arm on pillows.
- You will be advised to stretch your arm to workout the underarm. Most of lymph nodes are located in the armpit ( underarm) area. You may also be advised to lift the affected arm at shoulder height or above your head to restore the mobility and reduce chances of shoulder stiffness.
- Always inform the laboratory technician or nursing staff to prick the needle in the opposite arm for blood sample collection or medicine administering. Also blood pressure should be measured ( putting the blood pressure band) on the other arm.
- Protect against insect bites by using insect repellent (at least 50% DEET), and carry antiseptic cream for cuts and grazes.
- Limit your alcohol intake.
- Keep you arm clean and moisturized.
- Avoid wearing too tight sleeved clothes.
- If you’re travelling to a country where quick access to good-quality medical care is difficult, ask your GP for a course of antibiotics to take with you in case of infection. If you develop signs of infection in your ‘at risk’ arm or hand, treat the infection as early as possible, even if there’s no swelling.
Diagnosis of breast cancer treatment related lymphedema (BCRL):
Following diagnostic procedures are employed to diagnose a BCRL.
- Sequential circumferential arm measurements.
- Water displacement.
- Infrared Perometry.
- Bioelectrical impedance analysis.
Management of breast cancer treatment lymphedema (BCRL):
Once the BCRL is established in a breast cancer treated patient , there is nothing like a complete cure currently but providing symptomatic relief and avoiding complications of BCRL are the objectives of BCRL management. Management of lymphedema focuses on swelling reduction and symptom alleviation while minimizing exacerbations of swelling. Treatments include pharmacological therapy, surgery, complete decongestive physiotherapy (CDT), mechanical pneumatic pumps, and infection prevention and treatment.
Following procedures are employed for helping the BCRL patients.
- Pharmacological management of lymphedema uses benzopyrones, flavonoids, diuretics, hyaluronidase, pantothenic acid, and selenium.
- Surgical treatment for lymphedema includes microsurgical lympho-venous or lympho-lymphatic anastomoses, debulking, and liposuction.Surgery does not cure lymphedema, use of compression is necessary after surgery. Surgery for treatment of BCRL have it's owns cons like recurrence of swelling, poor wound healing, and infection. Surgical treatment should only be considered when other treatments fail, and with careful consideration of the benefits to risks ratio.
- Chronic lymphedema leads to formation of excess subcutaneous adipose tissue secondary to slow or absent lymph flow.Liposuction can help to remove excess fat tissue.Liposuction increases skin capillary blood flow without further damaging already compromised lymph transport capacity in breast cancer survivors with lymphedema. Patients are able to maintain limb size reduction with the use of compression garments after liposuction. Liposuction does not correct inadequate lymph drainage and is contradictory when pitting edema is present.
- Complete decongestive therapy (CDT) is the standard care for lymphedema.This approach includes manual lymph drainage, multi-layer, short-stretch compression bandaging, gentle exercise, meticulous skin care, education in lymphedema self-management, and elastic compression garments.
( This information is copied from Breast cancer-related lymphedema: Symptoms, diagnosis, risk reduction, and management
Mei R Fu)
Fu MR. Breast cancer-related lymphedema: Symptoms, diagnosis, risk reduction, and management. World J Clin Oncol 2014; 5(3): 241-247 [PMID: 25114841 DOI: 10.5306/wjco.v5.i3.241])
Feel free for any clarification or getting opinion from the best Indian breast cancer treatment specialists. You can send your queries to us on WhatsApp no: +91 9582056061.